Telemedicine App Development for Modern Healthcare
Building a telemedicine app is about more than just code. It’s the intricate process of creating a secure, intuitive, and compliant digital bridge connecting patients with their doctors for remote care. This involves a deep dive into feature planning, a non-negotiable commitment to regulations like HIPAA, and selecting a tech stack that can reliably deliver care from anywhere.
A successful app is built on a solid blueprint – one that carefully balances market needs with the realities of clinical workflows.
Your Blueprint for Modern Telemedicine App Development
The move to virtual healthcare isn’t just a fleeting trend; it’s here to stay. That’s why your telemedicine app needs a rock-solid plan from day one. This blueprint has to perfectly align with what the market wants, what users expect, and what regulators demand. After years of building healthcare software, we’ve seen firsthand that a well-defined strategy is the single most critical factor for success.

Whether you’re a startup looking to disrupt the industry or an established enterprise aiming to modernize, this guide provides a clear roadmap. We’ll break down the entire journey, from the initial brainstorming sessions to launching a secure and scalable platform. Think of this as the foundation: get this right, and everything else falls into place.
The Opportunity Is Real
The appetite for virtual care is undeniable. It represents a fundamental shift in how people access and receive medical attention. The global telemedicine market is forecasted to hit an incredible USD 124.01 billion in 2026 and is expected to climb to USD 532.08 billion by 2034. That’s not just growth; it’s an explosion of opportunity. You can dive deeper into the global telemedicine market forecast here.
What’s fueling this massive expansion? It boils down to a few key drivers:
-
Patients Expect More: People are now accustomed to on-demand services in every part of their lives, and healthcare is no exception. They want convenience, speed, and control.
-
Technology Has Caught Up: Widespread high-speed internet, powerful smartphones, and secure cloud infrastructure have made high-quality virtual consultations a reality.
-
Regulations Are Adapting: Governments and insurance bodies are increasingly supporting telehealth, creating clearer paths for providers to offer and get paid for virtual services.
A great telemedicine platform is so much more than a video chat app with a medical logo. It’s a complete digital care ecosystem that makes healthcare more accessible, streamlines clunky administrative tasks, and ultimately leads to better health outcomes. The secret is to solve a genuine problem for a specific group, whether that’s helping patients manage chronic diseases from home or offering immediate access to urgent care.
Building such a platform involves navigating a complex landscape. This guide will walk you through every critical phase, from deciphering compliance rules to picking the right technologies. As we explored in our guide on the benefits and challenges of mobile healthcare applications, a thoughtful, strategic approach is your best defense against common pitfalls.
To help visualize the journey ahead, let’s break down the core development process into distinct phases.
Core Development Phases for a Telemedicine App
| Phase | Key Objective | Primary Focus Areas |
|---|---|---|
| 1. Discovery & Strategy | Define the product’s purpose, scope, and business goals. | Market research, competitor analysis, user personas, compliance strategy (HIPAA/GDPR), feature prioritization. |
| 2. Design & Prototyping | Create an intuitive and engaging user experience (UX) and user interface (UI). | Wireframing, mockup creation, interactive prototyping, user flow mapping, accessibility considerations. |
| 3. Development & Coding | Build the functional front-end and back-end of the application. | Tech stack selection, API development, database architecture, secure coding practices, feature implementation. |
| 4. Testing & QA | Ensure the application is secure, stable, and bug-free. | Unit testing, integration testing, performance testing, security audits, user acceptance testing (UAT). |
| 5. Deployment & Launch | Release the application to the target app stores and servers. | App Store/Google Play submission, server configuration, launch marketing support, initial user onboarding. |
| 6. Maintenance & Scaling | Provide ongoing support and plan for future growth. | Performance monitoring, bug fixes, feature updates, user feedback analysis, infrastructure scaling. |
Each of these phases is a critical building block. Skipping or rushing one can jeopardize the entire project, so a methodical approach is key.
Building a Compliant and Feature-Rich Platform
Before you even think about writing a single line of code, let's talk about the most critical piece of the puzzle: compliance. This isn't just a box-ticking exercise; it's the absolute foundation of your telemedicine platform. Getting this wrong can result in staggering penalties: HIPAA violations alone can cost up to $1.5 million per violation, and completely erode patient trust, which is something you can never get back.

The only way to do this right is to build security into the app's DNA from the very beginning. We call this a "security by design" approach. It means protecting sensitive patient data is a core architectural principle, not a feature you bolt on at the end.
Navigating the Regulatory Maze
If you're operating in the United States, the Health Insurance Portability and Accountability Act (HIPAA) is your rulebook. For anyone serving users in Europe, the General Data Protection Regulation (GDPR) is the law of the land. While they have their differences, they share a common soul: protecting data privacy, ensuring top-notch security, and demanding clear user consent.
So, how do you actually make your app compliant? It comes down to a few non-negotiable technical and administrative safeguards:
-
End-to-End Encryption (E2EE): Think of this as an unbreakable digital seal. All data, whether it's flying across the internet during a video call or sitting in your database, must be encrypted. If a breach happens, the data is just unreadable gibberish to outsiders.
-
Secure Cloud Hosting: You can't just use any cloud provider. You need a partner like AWS, Google Cloud, or Microsoft Azure that will sign a Business Associate Agreement (BAA). This is a legally binding contract confirming they also follow HIPAA's strict rules for protecting health information.
-
Robust Access Controls: Not everyone in your organization needs to see patient records. By implementing role-based access control (RBAC), you ensure that people can only access the information absolutely necessary for their jobs. It’s a simple, powerful way to minimize internal risks.
-
Comprehensive Audit Trails: Your system has to be a meticulous record-keeper. It must log every single interaction with protected health information (PHI): who accessed it, what they did, and when. This creates a transparent trail for security audits and accountability.
To really pressure-test your defenses, you need to bring in the experts. Finding the right partners for robust penetration testing for HIPAA compliance is a crucial step. These "ethical hackers" will find your weak spots before malicious actors do.
Security isn't a one-time setup; it's a continuous process of monitoring, testing, and updating. Your compliance strategy must evolve alongside emerging threats and regulatory changes to remain effective. We've gone deeper into the technical side of this topic, as we explored in our guide on HIPAA-compliant software development.
Defining Your Minimum Viable Product (MVP) Features
Once your compliance strategy is locked in, it’s time to decide what to build first. This is where the Minimum Viable Product (MVP) comes in. An MVP isn't a buggy, incomplete app; it's the most streamlined version of your product that solves a real, core problem for your first users. This approach gets you to market faster, lets you collect invaluable feedback, and prevents you from sinking money into features nobody actually wants.
A solid telemedicine MVP absolutely must have these core components:
-
Secure Patient & Provider Profiles: Clean, simple interfaces for patients and doctors to manage their information, check appointment history, and securely update details.
-
Real-Time Video Consultations: This is the heart of your app. The video connection has to be rock-solid, secure, and incredibly easy to launch, even for users with less-than-perfect internet.
-
Appointment Scheduling & Management: An intuitive calendar that lets patients see when a doctor is free, book a slot, and get automatic reminders so they don't miss it.
-
Secure In-App Messaging: A HIPAA-compliant chat for those non-urgent conversations, think follow-up questions, clarifying a prescription, or sharing lab results securely.
-
e-Prescribing (eRx): This is a game-changer. It gives providers the ability to send prescriptions electronically right to the patient’s pharmacy, which is not only convenient but also cuts down on errors from bad handwriting.
Nailing these fundamentals ensures your MVP delivers real value from day one. It's the kind of foundational work you want a skilled partner to handle, ensuring your platform is built on a scalable and secure architecture right from the start.
Giving Your App a Competitive Edge with AI
A functional MVP is a great start; it gets your foot in the door. But to stay in the game and truly lead, you need to innovate. The next big thing in telemedicine isn't just a better video link; it's about making every single interaction smarter, faster, and more predictive. This is exactly where artificial intelligence stops being a buzzword and becomes your biggest competitive advantage.

When you weave AI into your platform, it transforms from a simple communication tool into an intelligent health assistant. We've seen firsthand how these enhancements improve patient outcomes, lighten the load for providers, and create a much more valuable, "sticky" experience for patients.
The market is already screaming for this shift. The global AI in telehealth market is on a rocket ship trajectory, projected to explode from USD 3.89 billion in 2024 to an incredible USD 86.31 billion by 2034. This isn't just hype; it's driven by real user behavior. Think about it: 76% of U.S. adults who tried telemedicine in 2023 came back for more, which tells us they expect increasingly sophisticated virtual care.
Smarter Patient Triage and Support
One of the quickest wins with AI is right at the "front door" of your virtual clinic. Imagine an intelligent chatbot handling the initial patient intake. It can gather symptoms through a natural conversation, not a clunky form. This does more than just free up administrative time; it neatly structures all that crucial data for the clinician before the appointment even starts.
For instance, a patient mentioning chest pain gets immediately flagged for an urgent human review. On the other hand, someone with mild allergy symptoms might be automatically routed to a nurse practitioner or even get some helpful self-care resources. As we explored in our guide to AI chatbots in healthcare, these tools are game-changers for navigating patient flow efficiently.
Ultimately, this kind of smart triage makes sure your clinical team's time is spent where it matters most.
AI-Powered Clinical Decision Support
During a consultation, AI can act as a trusted co-pilot for the healthcare provider. By analyzing a patient's symptoms, medical history, and even live data streaming from connected wearables, AI algorithms can surface potential diagnoses or red-flag risk factors that need a closer look.
Here’s how this plays out in the real world:
-
Diagnostic Suggestions: A dermatologist could use an AI tool to analyze a high-res photo of a skin lesion. The tool would then present a list of probable conditions, ranked by likelihood, for the doctor to confirm.
-
Predictive Analytics: For a patient with diabetes, the system could analyze glucose trends from their remote monitor and send an alert to the provider about a rising risk of a hyperglycemic event, enabling proactive intervention.
-
Documentation Automation: Natural Language Processing (NLP) is a huge time-saver. It can listen to the patient-doctor conversation and automatically draft a structured clinical note (like a SOAP note), slashing the paperwork burden on providers.
The goal here isn't to replace a doctor's expertise. It's to supercharge it. AI provides data-driven insights that help clinicians make faster, more informed decisions, freeing them up to focus on the person, not just the problem. Leveraging AI for your business in this way creates immense value.
Beyond AI: Other High-Impact Integrations
To really pull ahead of the pack, think about pairing AI with other powerful features. Truly using artificial intelligence in healthcare effectively means making it part of a larger, seamless ecosystem.
Here are a few integrations that deliver massive value:
-
Seamless EHR/EMR Connectivity: This is non-negotiable. Information has to flow smoothly and securely between your app and a clinic’s Electronic Health Record system to ensure continuity of care.
-
Remote Patient Monitoring (RPM): Integrating with IoT devices, think smart scales, blood pressure cuffs, and glucose meters, unlocks continuous, real-time health data that was previously impossible to get.
-
Secure Payment Systems: A built-in, secure payment gateway makes life easier for everyone. It should effortlessly handle co-pays, subscription fees, or one-off visit charges without friction.
Putting these pieces together elevates your app from a standalone tool to a comprehensive digital health hub – one that patients and providers can't imagine living without.
Choosing Your Technology Stack and Development Team
Getting the technology right and putting the perfect team in place are two of the most make-or-break decisions you'll face when building a telemedicine app. Think of your tech stack as the engine of the whole platform; it dictates performance, security, and whether you can scale later on. Just as crucial is the team building that engine. Their skill and experience will directly shape the quality and ultimate success of your app.
These choices are foundational. A clumsy tech stack can create performance nightmares and force expensive rebuilds down the road. An unbalanced team can lead to frustrating delays and a user experience that falls flat. The magic happens when you get the technology and the talent working in perfect sync. Our own experience, which you can see in our client cases, proves time and again that this synergy is the secret to a successful launch.
Assembling Your A-Team
Building a telemedicine app isn't a job for a handful of coders; it's a complex mission that demands a wide range of expertise. You need a well-rounded team where every part of the project, from the first design sketch to server maintenance, is handled by someone who truly knows their stuff. This goes far beyond just writing code; it requires a strategic mix of roles to navigate the unique challenges of healthcare software development.
Here are the key players you'll need on your bench:
-
Project Manager (PM): This is your team's conductor. They keep the project moving on schedule, on budget, and in line with your business goals. A good PM is a master communicator who clears roadblocks before they become problems.
-
UI/UX Designer: Absolutely critical. This person is responsible for making the app intuitive and easy to use for both patients and doctors. They design the entire user journey, ensuring it’s accessible to everyone, regardless of their tech-savviness.
-
Backend Developers: The architects behind the scenes. They build and maintain the server, database, and APIs – the core logic that handles everything from secure logins to patient data storage.
-
Frontend Developers (Web/Mobile): These are the experts who bring the UI/UX designs to life. They build the interactive parts of the app that people actually see and use. You’ll likely need specialists for web, iOS, and Android.
-
QA Engineers: Your last line of defense against bugs. These detail-oriented testers put the application through its paces, finding and reporting issues before they ever reach your users. They ensure a polished, reliable final product.
-
DevOps Engineer: This role is the bridge between development and IT operations. They manage the cloud infrastructure, automate deployments, and make sure the platform is secure, stable, and ready to grow.
Crafting the Ideal Technology Stack
Picking your tech stack is a lot like choosing the materials to build a house. You need the right combination of tools to create something sturdy and reliable. Your stack is generally broken down into the frontend (what users see), the backend (the server-side brain), and the infrastructure that supports it all.
Here’s a piece of hard-won advice: the best tech stack isn't always the newest or flashiest. It's the one that fits your specific needs, your team's skills, and your long-term goals. Focus on stability, security, and scalability; not just the latest trend.
To give you a clearer picture, let's explore a sample tech stack that balances high performance with the rock-solid security a telemedicine platform demands.
Sample Technology Stack for a Telemedicine Platform
The table below outlines common technology choices for each part of a telemedicine app. The "right" choice always depends on your project's unique requirements, from real-time communication needs to data processing demands.
| Component | Technology Options | Key Considerations |
|---|---|---|
| Frontend (Web) | React, Angular, Vue.js | React has a massive community and library support. Angular is a more structured, all-in-one framework. Vue.js is often praised for its simplicity and ease of learning. |
| Frontend (Mobile) | Swift (iOS), Kotlin (Android), React Native | Native (Swift/Kotlin) delivers the absolute best performance and device integration. React Native is a great option for building for both iOS and Android faster with a single codebase. |
| Backend | Node.js, Python (Django), Ruby on Rails | Node.js excels at real-time features like chat and video. Python is a powerhouse for data science and AI. Rails is known for enabling very rapid development. |
| Database | PostgreSQL, MySQL, MongoDB | PostgreSQL and MySQL are reliable relational databases, perfect for structured medical data. MongoDB is a flexible NoSQL option for less structured information. |
| Cloud Infrastructure | AWS, Microsoft Azure, Google Cloud Platform (GCP) | All three giants offer HIPAA-compliant services and will sign a Business Associate Agreement (BAA). The best fit often comes down to specific services or team familiarity. |
| Video & Chat APIs | WebRTC, Twilio, Agora | WebRTC is an open-source standard giving you total control. Twilio and Agora are third-party services that offer reliable, pre-built video/chat infrastructure to speed up development significantly. |
Ultimately, these tools are just means to an end. The goal is to select a stack that is secure, compliant, and won't hold you back as your platform grows.
In-House vs. Outsourcing: A Strategic Decision
With your roles and tech defined, the final big question is: who will build it? Do you hire a team in-house or partner with an outside agency? There’s no single right answer; it really comes down to your budget, timeline, and what you want for the future.
Building an in-house team gives you complete control and allows you to grow deep product knowledge over time. The downside is that it's a slow and expensive process, filled with recruiting, hiring, and onboarding.
On the other hand, outsourcing to a partner specializing in custom software development gives you instant access to a complete, experienced team. This route is typically faster and more cost-effective, letting you tap into specialized skills without the long-term overhead. It’s a powerful strategy to get your project off the ground quickly and with proven expertise from day one.
The Development Lifecycle: From MVP to Launch
Taking your telemedicine app from a concept on paper to a live product in the hands of users is a disciplined journey. It's not a single mad dash to the finish line; it’s a series of deliberate, well-managed phases. Think of it as methodically translating your vision into a blueprint (wireframes), then building a solid foundation (the MVP), and finally, polishing it into a market-ready application.
This structured approach is crucial. It ensures every feature has a purpose, every line of code is solid, and the final experience is seamless for both patients and clinicians. It’s the proven path from an idea to a reliable, real-world tool.
From Discovery to Interactive Prototypes
Before a single line of code gets written, we have to lay the groundwork in the discovery and design phase. This is where we turn business goals and user needs into a tangible plan. We start with wireframes – simple, black-and-white outlines of the app. They act like a skeleton, mapping out user journeys and core structure without the distraction of colors or fonts.
Once we agree on the flow, we build high-fidelity mockups and interactive prototypes. These are far more than static images; they are clickable, tappable models that look and feel like the real app. This gives stakeholders a chance to actually use the app and provide feedback on its usability long before development costs start to add up. It's a "test before you build" philosophy that is the cornerstone of efficient custom software development, saving a ton of time and money by catching design issues early.
This flow chart gives a bird's-eye view of how a telemedicine app comes to life, from choosing the right technology to getting the right people on board.
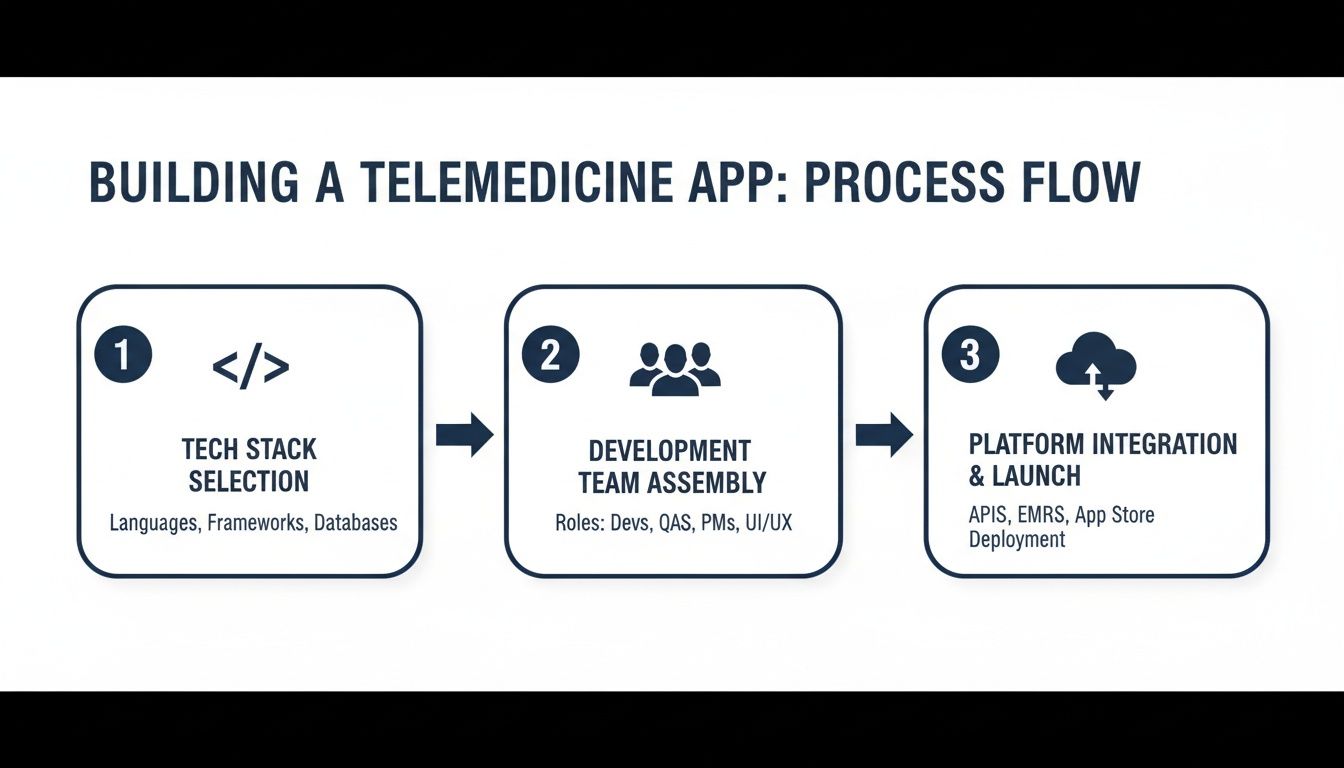
As you can see, successful development hinges on two things: a solid tech foundation and a skilled team that can bring the vision to life.
Agile Sprints and MVP Construction
With a validated design locked in, we jump into development, and the best way to manage this is with an agile methodology. We don’t try to build the whole thing at once. Instead, we break the project into small, manageable chunks called "sprints," which usually last two weeks. In each sprint, we commit to building and testing a specific set of features from our list.
The first major goal is building the Minimum Viable Product (MVP). This isn't a stripped-down, cheap version of your app. It's the leanest version that solves the core problem for your first users, containing only the absolute must-have features, things like secure video calls, basic appointment scheduling, and patient profiles.
Building an MVP first is a strategic move. It gets your product to market faster, lets you collect invaluable feedback from real users, and helps you validate your core ideas without sinking a huge investment into features people might not even want. This iterative cycle minimizes risk and makes sure the product is shaped by the market, not just by assumptions.
This agile approach keeps the momentum going and allows us to be flexible. At the end of every sprint, we demonstrate what we've built, get feedback, and adjust priorities for the next sprint. This keeps the project on track and aligned with your business needs as they evolve.
Comprehensive Testing and Quality Assurance
In healthcare, trust is everything. A buggy or unreliable app can shatter that trust in an instant. That’s why rigorous testing isn't an afterthought; it’s baked into the entire development process. Our QA engineers work side-by-side with developers in every sprint, making sure each new piece of functionality is rock-solid.
Our testing protocol is multi-layered, leaving no stone unturned.
-
Functional Testing: We make sure every button, workflow, and feature works exactly as designed. No surprises.
-
Performance Testing: We push the app to its limits to ensure it can handle a heavy load of users without crashing or slowing down, especially during peak times.
-
Security Testing: This is non-negotiable. We actively try to break in, running penetration tests and vulnerability scans to ensure patient data is locked down and fully HIPAA/GDPR compliant.
-
Usability Testing: We put the app in front of real users to get their honest feedback, confirming it’s intuitive and easy for everyone to navigate.
Deployment, Maintenance, and Future Growth
Going live isn't the end of the road; it’s just the beginning. The deployment phase involves packaging the app and carefully submitting it to the Apple App Store and Google Play Store, both of which have their own strict rules to follow. At the same time, we get the backend up and running on secure, scalable cloud servers.
Once your app is live, our focus shifts to keeping it healthy and growing.
-
Performance Monitoring: We keep a close eye on the app's stability, speed, and uptime.
-
Bug Fixes: When issues pop up from real-world use, we jump on them quickly.
-
User Feedback Analysis: We dive into user reviews, support tickets, and usage data.
This constant stream of feedback is gold. It fuels a data-driven roadmap for future updates and new features, ensuring your telemedicine app doesn't just launch, but evolves to meet the needs of your users and stay ahead of the competition.
What’s the Real Cost and Timeline for Building a Telemedicine App?
Let’s talk numbers. When you're planning a telemedicine app, getting a handle on the budget and timeline is everything. There’s no single price tag; of course, the final cost is a direct reflection of your ambition. The biggest factors that will move the needle are the app's complexity, the number of features you need, and whether you're building for one platform or several.
A straightforward app for just iOS, for example, is a much smaller financial lift than a sophisticated system that works across iOS, Android, and the web. Every advanced feature you add, like an AI-powered symptom checker or deep integration with a dozen different EHR systems, will naturally add to both the cost and the development clock.
Breaking Down the Budget
To give you a realistic starting point, it helps to think about projects in tiers. These aren't set in stone, but they provide a solid framework for what to expect based on the scope you’re aiming for.
-
A Lean MVP (Minimum Viable Product): This is your launchpad. It includes the absolute must-haves: secure video calls, basic scheduling, and simple user profiles. Think of it as getting the core functionality right first. You're typically looking at a range of $75,000 to $125,000.
-
A Comprehensive Platform: Here, we're building a more polished and powerful tool. This usually involves seamless EHR integration, e-Prescribing capabilities, and a custom-designed user experience for both web and mobile. The budget for this level generally lands between $150,000 and $300,000.
-
An Enterprise-Grade Solution: This is the all-in-one platform built for scale. It supports multiple medical specialties, features advanced data analytics, incorporates AI/ML, and connects with a wide array of third-party services. These complex projects often start at $300,000 and go up from there.
Keep in mind, these aren't just development costs. They cover the entire journey, from the initial discovery and design sessions to rigorous testing and the final launch. Investing properly upfront in a compliant, well-thought-out architecture is the best way to avoid expensive overhauls down the road.
Mapping Out the Development Timeline
Just like the budget, the timeline is all about the scope. A good development process has a natural rhythm, with each phase setting the stage for the next. Trying to rush key stages like discovery or security testing is a classic mistake that almost always ends up causing bigger delays and surprise costs later.
Here’s what a typical timeline for a comprehensive telemedicine platform looks like:
| Phase | Estimated Timeline | What Happens Here |
|---|---|---|
| Discovery & Design | 4-6 Weeks | We dig into requirements, map out compliance strategy, design the user experience, and build prototypes. |
| Development & Integration | 12-20 Weeks | This is where the code comes to life: building the front and back ends, developing APIs, and connecting to EHRs. |
| Testing & Deployment | 4-6 Weeks | We hunt for bugs, conduct security audits, validate compliance, and finally, launch the app to the world. |
All in, you’re looking at an average of 6 to 8 months from start to finish. This gives you a clear picture of the commitment involved. Partnering with an experienced AI solutions partner who knows this terrain can make all the difference, ensuring you hit every milestone with confidence.
Frequently Asked Questions (FAQ)
What features are essential for a telemedicine app MVP?
A Minimum Viable Product (MVP) should focus on the core functionality that solves the primary problem for your users. For a telemedicine app, these essentials include secure patient and provider profiles, real-time video and audio consultations, a basic appointment scheduling system, secure in-app messaging, and e-Prescribing (eRx) capabilities. Starting with these features allows you to launch faster, gather user feedback, and validate your concept before investing in more advanced functionalities.
How do I ensure my telemedicine app is HIPAA compliant?
HIPAA compliance must be a foundational part of your development strategy, not an afterthought. Key technical requirements include end-to-end encryption for all data (in transit and at rest), secure cloud hosting with a provider that offers a Business Associate Agreement (BAA) like AWS or Azure, robust access controls (RBAC), and comprehensive audit trails that log all interactions with Protected Health Information (PHI). Engaging in regular security audits and penetration testing is also crucial.
How much does it cost to develop a telemedicine app?
The cost varies significantly based on complexity, features, and the number of platforms (iOS, Android, web). A basic MVP can range from $75,000 to $125,000. A more comprehensive platform with EHR integrations and custom UI/UX typically falls between $150,000 and $300,000. An enterprise-level solution with advanced features like AI-powered diagnostics and analytics can exceed $300,000. These estimates should cover the entire process, from discovery and design to development, testing, and launch.
How long does telemedicine app development take?
The timeline is directly tied to the project’s scope. A typical project can be broken down into phases: Discovery & Design (4-6 weeks), Development & Integration (12-20 weeks), and Testing & Deployment (4-6 weeks). On average, you can expect a comprehensive telemedicine app to take between 6 and 8 months from the initial concept to a market-ready launch. Building an MVP first can significantly shorten the initial time to market.
Should I build an in-house team or outsource development?
This is a strategic choice based on your resources and goals. Building an in-house team offers maximum control but is often slow and costly. Outsourcing to a specialized firm that provides custom software development services gives you immediate access to a full team of experts, which is often faster and more cost-effective. A specialized partner brings proven experience in complex areas like healthcare software development and HIPAA compliance, reducing risk and accelerating your timeline.



