A Practical Guide to FHIR Integration for Healthcare
FHIR integration is all about using the Fast Healthcare Interoperability Resources (FHIR) standard to get different healthcare systems talking to each other. Think of it as a universal translator for clinical and administrative data, using modern web APIs to finally break down the walls between electronic health records (EHRs), patient portals, and all sorts of digital health apps. It creates a common language, ensuring data can move seamlessly and securely across the entire healthcare ecosystem.
Why FHIR Integration Is No Longer Optional
In the tangled mess of healthcare technology, FHIR isn't just another buzzword; it's become the essential language for modern, connected care. For decades, providers and payers have been hamstrung by data locked away in proprietary systems, which makes getting a complete picture of a patient's health nearly impossible. FHIR tackles this problem head-on by creating a standardized pathway for information to flow freely and securely between systems that otherwise couldn't communicate.
This shift from a fragmented landscape to a truly interconnected one is already changing how clinicians work and improving patient outcomes. Imagine a cardiologist instantly pulling up a patient's full medical history from their primary care doctor's EHR, or a patient using a single mobile app to gather their lab results from three different facilities. This isn't science fiction; it's the practical reality that FHIR makes possible today.
Before we dive into the technical "how-to," it helps to have a solid grasp of the core concepts that make FHIR work. This table breaks down the essentials.
Key FHIR Concepts at a Glance
| Concept | Description | Real-World Example |
|---|---|---|
| Resource | The fundamental building block of FHIR. It's a structured packet of information about a specific healthcare entity. | A Patient Resource contains demographic data like name, date of birth, and address. A MedicationOrder Resource details a prescription. |
| Profile | A set of rules or constraints applied to a base Resource to adapt it for a specific use case or region. | The US Core Patient Profile adds requirements for race and ethnicity to the base Patient Resource to meet US regulatory needs. |
| RESTful API | FHIR uses REST (Representational State Transfer) principles for its API, allowing systems to interact using standard web commands. | A client application would use an HTTP GET request to [FHIR_Server_URL]/Patient/123 to retrieve the record for the patient with ID 123. |
| JSON/XML | The data formats used to represent FHIR Resources. JSON (JavaScript Object Notation) is the more common and human-readable format. | A Patient Resource sent over the API would be formatted as a JSON object with key-value pairs like "given": ["John"] and "family": "Doe". |
Understanding these pieces is the first step toward building robust, interoperable solutions. They are the foundation upon which all FHIR-based communication is built.
The Market and Regulatory Push
The push toward universal FHIR integration is coming from all sides, driven by both market demands and government regulations. Patients expect instant access to their health data, and providers need that information in real-time to make critical decisions. As a result, seamless data exchange has moved from a nice-to-have feature to a competitive must-have.
The numbers tell the story. In the US outpatient market alone, FHIR app adoption shot up from 49% in 2021 to 64% in 2024, a 30% relative jump in just three years. The global trend is even stronger, with 71% of organizations expected to be using FHIR in their day-to-day operations by 2025. This isn’t a slow burn; it’s a tipping point. If you want to partner with anyone in the digital health space, you need to speak FHIR. You can explore the full EHR adoption statistics on Aptarro.com to see just how fast the landscape is changing.
FHIR’s real power is its ability to unlock innovation. By creating a standard data layer, it provides the key to advancing analytics, AI-powered diagnostics, and truly personalized medicine.
For any organization navigating this shift, the technical hurdles can be steep. A successful FHIR implementation demands deep expertise in both healthcare data standards and modern software architecture. This is where finding an experienced AI solutions partner becomes critical, especially for those in specialized areas like healthcare software development. Getting the right help ensures your implementation is not only compliant and scalable but also built to handle whatever comes next.
Choosing the Right FHIR Integration Architecture
Picking the right FHIR integration architecture is like drawing the blueprint for a new building. Every decision you make at this stage, from the foundation up, is going to define the stability, scalability, and everyday usefulness of the final product. This isn’t about finding a single “best” method. It’s about digging in and finding the best pattern for your specific situation, considering your existing systems, future goals, and the problems you’re actually trying to solve.
The journey usually starts with one big question: are you connecting to a system that already speaks FHIR, or are you building a bridge to an older, legacy system? The answer sets the course for your entire project.
Direct API Layer vs. Adapter Engine
A direct API layer is the dream scenario. It’s clean, efficient, and the most straightforward path forward. You’d go this route when connecting to a modern EHR or any platform that has a native FHIR API. Your application simply talks directly to the system’s FHIR endpoint, using its built-in capabilities to exchange data.
This approach means faster development and less initial complexity. Think of a new patient-facing app pulling lab results from a hospital’s modern EHR. With a direct API, there’s no need for a middleman to translate the conversation.
But let’s be realistic – healthcare is full of critical systems that were built long before FHIR came along. This is where an adapter or mapping engine becomes your most valuable tool. This architecture acts as an interpreter, sitting between your app and the legacy system. It takes a FHIR request, translates it into something the old system understands (like an HL7v2 message or a specific database query), and then translates the response back into a standard FHIR resource.
Sure, it adds a layer of complexity, but it’s a game-changer for unlocking data from systems that would otherwise be information silos. A classic use case is integrating a new telehealth platform with several different hospitals, each running its own aging, non-FHIR EHR. The adapter is the key to making that work.
The core architectural choice comes down to this: are you tapping into an existing FHIR stream, or are you creating a new one from a non-FHIR source? The answer dictates your entire integration strategy.
This decision-making process is really about assessing your current state and future needs.
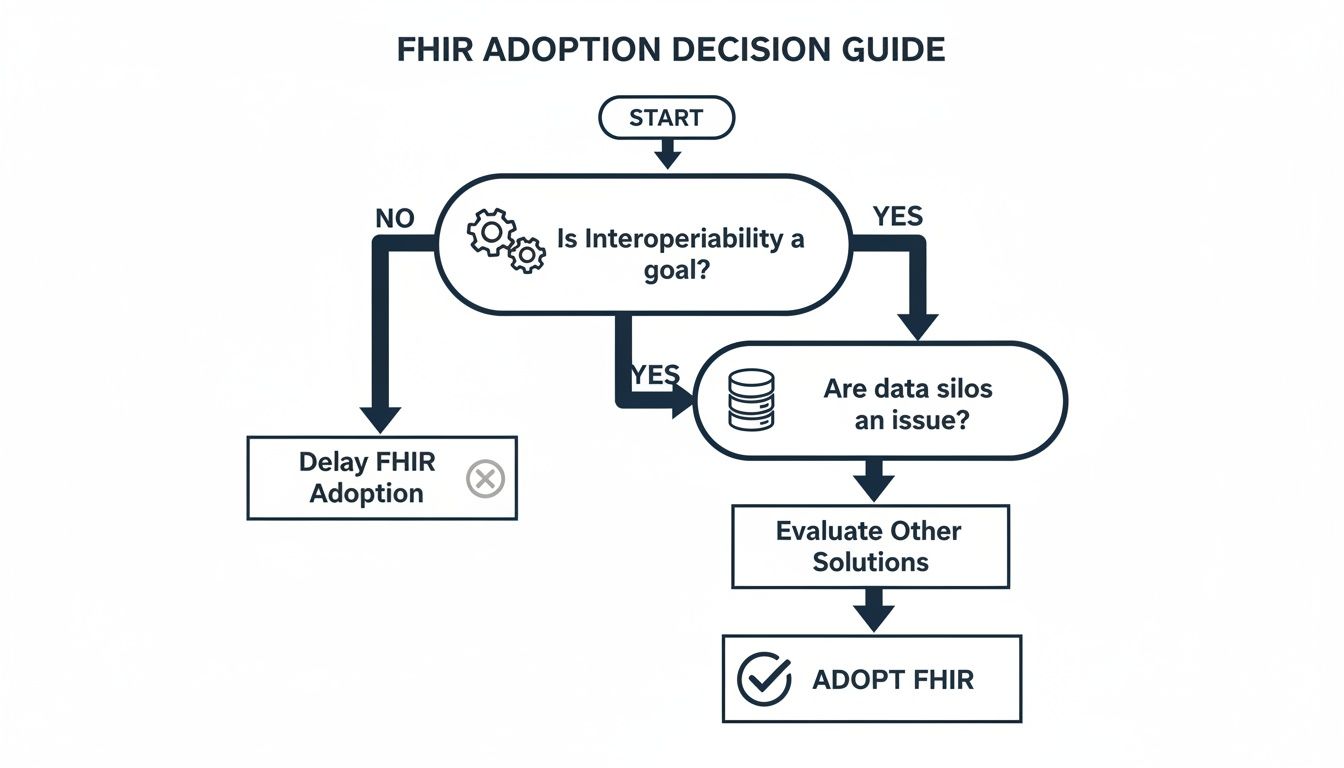
As the chart shows, if you’re aiming for true interoperability and battling fragmented data, FHIR isn’t just a nice-to-have. It’s a strategic necessity.
RESTful vs. Message-Based Communication
Once you know how you’re connecting, the next piece of the puzzle is deciding how the data will actually move. The two main patterns here are RESTful and message-based.
RESTful (Synchronous)
This is what most people think of when they talk about FHIR. It uses the standard web language of HTTP methods: GET, POST, PUT, DELETE, for real-time, on-demand data requests. It’s a synchronous, “ask and wait” model. Your application sends a request and waits for an immediate response.
This is perfect for interactive scenarios. A doctor pulling up a patient’s allergy list in the middle of an appointment is a prime example. The exchange is immediate and happens right in the workflow.
Message-Based (Asynchronous)
On the other hand, a message-based approach is built for workflows where an immediate response isn’t necessary, or for broadcasting information to multiple systems at once. A system publishes a FHIR message (usually a Bundle of resources) to a message queue, and other systems can subscribe and grab it when they’re ready.
For instance, when a patient is discharged, the EHR could publish a “discharge summary” message. The billing department, the patient’s primary care provider, and a home health agency can all pick up that message on their own time. This decouples the systems, making the whole network more resilient if one part goes down.
In practice, the most robust solutions often use a hybrid model. You might use RESTful APIs for real-time clinical lookups, but rely on a message-based system for administrative tasks like broadcasting patient registration updates. Understanding how to connect these disparate parts is crucial, and as we explored in our guide, you can learn more about the bigger picture with these hospital system integration services. Getting the architecture right from the start means you’re building something that not only works today but is also ready for whatever comes next.
Getting Your Hands Dirty with FHIR Data Modeling and Mapping
If your architecture is the plumbing of your FHIR integration, then data modeling is the water flowing through it. This is where the rubber meets the road, translating your system’s unique data language into the universal dialect of FHIR. Honestly, this is often the most painstaking part of the entire project, a deep dive where technical precision meets the messy reality of clinical data.
The whole game is about converting your existing data models, which might be in a proprietary database format, into standard FHIR Resources. Think of these resources as the nouns of healthcare: Patient, Observation (like a blood pressure reading), Encounter (a doctor’s visit), and so on.
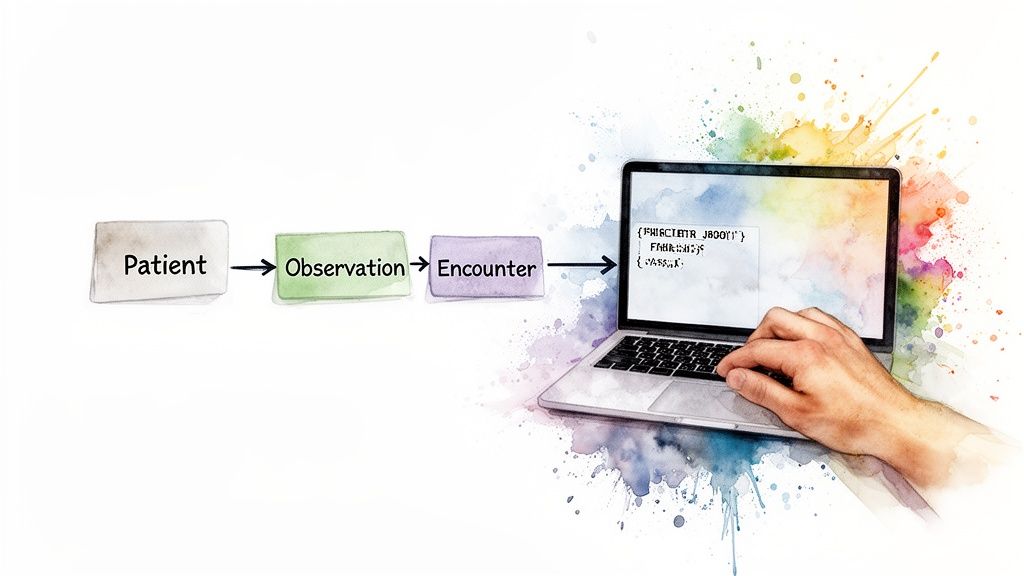
From Custom Tables to Standard Resources
Let’s get practical. Say your old database has a custom table for blood pressure with columns like BP_Systolic and BP_Diastolic. You can’t just dump that into FHIR. Instead, you create a proper Observation Resource.
This is more than a simple copy-paste. You have to populate the FHIR structure with the right context:
-
status: Set to ‘final’ to show it’s a confirmed reading. -
category: Classify it as ‘vital-signs’. -
code: Use a standard LOINC code, like ‘85354-9’, for the overall blood pressure panel. -
subject: Link it back to the specificPatientResource. -
component: This is crucial. Create an array with separate components for systolic (LOINC ‘8480-6’) and diastolic (LOINC ‘8462-4’) values.
By doing this, you’re not just moving data; you’re adding layers of standardized meaning so any other FHIR-compliant system knows exactly what it’s looking at. This kind of detailed transformation is at the heart of any serious custom software development effort in healthcare.
What About Our Unique Data? Profiles and Extensions to the Rescue
The base FHIR specification is great, but it only covers about 80% of what you’ll find in the wild. What about that last 20%? Every hospital, clinic, and lab has its own quirky data fields, local coding systems, or workflow-specific needs.
This is where you bring in FHIR Profiles and Extensions. They are your tools for tailoring FHIR without breaking it.
A Profile is like a blueprint that adds rules to a base FHIR resource. A fantastic example is the US Core Patient Profile, which makes elements like race and ethnicity mandatory for a Patient Resource, even though they’re optional in the global standard.
An Extension, on the other hand, lets you add completely new information. Need to store a patient’s preferred contact method, like “text message”? The base Patient Resource doesn’t have a field for that. No problem, you just add it as a custom extension.
The genius of FHIR is this balance between a rigid standard and practical flexibility. With Profiles and Extensions, you can meet specific local or regulatory demands while ensuring your core data remains interoperable with the rest of the world.
The Importance of Speaking the Same Language with Terminology Services
Mapping the fields is only half the battle. The values inside those fields need to mean the same thing everywhere. This concept is called semantic interoperability, and it’s powered by standardized terminologies.
This is where Value Sets come into play. A Value Set is just a pre-approved list of codes for a specific field. For instance, the gender element might be restricted to a Value Set containing ‘male’, ‘female’, ‘other’, and ‘unknown’.
Using industry-standard code systems is non-negotiable. We’re talking about:
-
SNOMED CT for clinical findings and diagnoses
-
LOINC for lab tests and observations
-
RxNorm for medications
This practice ensures that when your system sends a code for “myocardial infarction,” every receiving system understands it’s a heart attack, with no room for misinterpretation.
Don’t Forget Validation and Versioning
Once you’ve mapped everything, how do you know you got it right? You validate it.
FHIR comes with validators – tools that check your newly created resources against the base spec and any profiles you’ve applied. This absolutely must be an automated step in your CI/CD pipeline. Catching a data formatting error before it hits production can save you from a world of hurt. As we’ve noted before, poor data quality is one of the biggest challenges in hospital integration.
Finally, you have to think about FHIR versions. The standard evolves (e.g., from R4 to R5), and you’ll inevitably find yourself needing to connect with systems running on different versions. A robust architecture plans for this. You might need to support multiple versions at once or build a clear process for migrating data between them. This kind of forward-thinking is what separates good from great in healthcare software development.
Building a Secure and Compliant FHIR Implementation
In healthcare, data security is more than just a best practice; it’s the law, and it’s the foundation of patient trust. A FHIR integration is only as good as its security framework. Without rock-solid protections, even the most innovative system is a massive liability. This is the crucial step where you move from building something that works to building something that is trustworthy.
The bedrock of modern FHIR security is the powerful combination of OAuth 2.0 and the SMART on FHIR framework. Think of OAuth 2.0 as the bouncer at the club, handling the fundamental job of verifying identity and granting access. It’s the industry-standard protocol for secure authorization across the web.
SMART on FHIR then takes that solid foundation and tailors it specifically for the unique demands of healthcare. It creates a standardized, open-source security layer that lets third-party apps connect securely to EHRs and other health data systems. This is the magic that allows a clinician to launch, say, a specialized cardiology app directly from their EHR workflow. The app gets the right context, like which patient’s record is open, without a clumsy or insecure data handoff.
Mastering Authentication and Access Control
True security for your FHIR integration comes down to one thing: ensuring only the right people access the right data for the right reasons. This goes way beyond a simple username and password. It requires a layered, deliberate approach to authentication and authorization.
The typical flow is designed for maximum security:
-
Request: A third-party app needs patient data from the EHR’s FHIR server.
-
Authentication: The user (a clinician, for instance) is sent to a secure authorization server to log in and prove who they are.
-
Permission: The user grants the app-specific permissions, known as “scopes.” This could be permission to read patient demographics but not to write new data.
-
Token: The authorization server issues a secure access token to the app. This token is a temporary key with a limited lifespan and a specific purpose.
-
API Calls: The app includes this token with every request it makes to the FHIR server, which validates it every single time before returning any data.
This token-based system is absolutely critical. It means the app never stores the user’s actual credentials, which dramatically shrinks the potential attack surface.
At its core, SMART on FHIR provides a “plug-and-play” security model. It standardizes the complex handshake between applications and data sources, allowing developers to focus on building valuable clinical tools instead of reinventing the security wheel for every new EHR they connect with.
Ensuring Compliance Through Auditing and Logging
Meeting regulations like HIPAA is a non-negotiable part of any FHIR project. While the FHIR standard itself isn’t inherently HIPAA-compliant, it gives you all the tools you need to build systems that are. A core requirement here is the ability to track and audit every single interaction with protected health information (PHI).
Your FHIR server must maintain meticulous logs of all API activity. This isn’t just for debugging; it’s a critical compliance instrument. These audit trails need to capture the essentials:
-
Who accessed the data (which user and which application).
-
What data they accessed (the specific FHIR resources and patient IDs).
-
When it happened (a precise timestamp).
-
Where the request came from.
-
The outcome of the request (success or failure).
These logs are your proof of compliance. They show you have complete visibility and control over PHI and are indispensable for security audits, investigating potential breaches, and satisfying legal requirements. As we’ve covered in our guide, building systems that meet these strict rules is fundamental to all HIPAA-compliant software development.
Ultimately, a secure and compliant FHIR implementation isn’t something you tack on at the end. It has to be woven into the architecture from the very first line of code. This commitment to security is what ensures that innovation never comes at the expense of patient privacy.
Making Your FHIR System Fast, Reliable, and Ready to Scale
A FHIR integration that just works isn’t enough. It has to perform reliably under pressure and scale smoothly as your data and user traffic grow. A slow, brittle API isn’t just a technical headache; it directly hinders patient care and frustrates clinicians. This is where we move past the theory and get into the real-world nuts and bolts of building a system that’s fast, resilient, and built for the future.
The pressure for high-performance systems is only increasing. By 2026, FHIR integration is expected to be a global standard, driven by major regulations like the CMS Interoperability and Prior Authorization Final Rule. This isn’t some far-off prediction; in the US, 70% of non-federal acute care hospitals are already deeply engaged in interoperability, and clinicians report using external data at the point-of-care 70% of the time. This shows just how critical a well-built, scalable FHIR system is to modern healthcare. For a closer look at these trends, you can explore the healthcare interoperability predictions on HealthcareITToday.
Designing for Speed and Scale from Day One
You can’t just add “performance” later on. It has to be woven into your architecture from the very beginning. From my experience, three strategies are non-negotiable for a high-performance FHIR API: smart caching, robust load balancing, and meticulous database indexing.
Caching, Load Balancing, and Indexing
-
Smart Caching: Think about how often a clinician pulls up the same patient’s allergy list or demographics. Many FHIR requests are repetitive. By caching this frequently accessed, relatively static data, you can serve these common requests in milliseconds instead of hitting your database every time. Tools like Redis are perfect for creating this kind of high-speed caching layer, drastically reducing server load and making the user experience feel instantaneous.
-
Load Balancing: A single server can only handle so much. As your application gains users, you’ll need a load balancer to act as a traffic director, intelligently distributing incoming API requests across a pool of servers. This not only prevents any one server from becoming a bottleneck but also ensures your system stays available even if one server goes down. It’s the key to scaling out horizontally.
-
Database Optimization: At its core, a FHIR server is a highly specialized database, and slow queries are the number one killer of API performance. You absolutely must properly index your database on the FHIR parameters that will be searched most often, things like patient identifiers, observation codes, or encounter dates. An index allows the database to find records almost instantly, avoiding the painful process of scanning millions of rows for every query.
A well-tuned FHIR system should feel invisible to the end user; it just works. The ultimate goal is to make data access so fast and reliable that clinicians don’t even have to think about it.
The Power of Sandboxes and Rigorous Testing
You wouldn’t test a new medical device on a live patient, and the same logic applies to your FHIR integration. This is where FHIR sandboxes come in. These are isolated environments that mimic a production system but use safe, synthetic data. They are an absolute must-have for any serious development effort.
A good sandbox lets your team:
-
Innovate Safely: Developers get a place to experiment, break things, and fix them without ever touching real patient data or disrupting clinical workflows.
-
Validate Conformance: You can test your app’s compliance with FHIR standards and specific implementation guides long before you attempt to connect to a live EHR.
-
Stress Test Your System: Want to know how your system will handle a thousand concurrent users? A sandbox is the place to run load tests, find bottlenecks, and fine-tune your scaling strategy.
This cycle of rigorous testing is a cornerstone of building dependable software. As we’ve discussed in our guide to digital health platform engineering, adopting a “test-first” mindset can prevent countless headaches down the road. In fact, our own client cases consistently show that projects with a strong emphasis on testing have far smoother launches and better long-term stability.
Essential Tools for Your FHIR Implementation
Navigating the FHIR ecosystem means knowing what tools are available to help you build, test, and deploy your solutions. The right tooling can save your team hundreds of hours and ensure your implementation is robust and compliant. Here’s a look at some of the key tools development teams rely on.
| Tool Category | Examples | Key Use Case |
|---|---|---|
| FHIR Servers | HAPI FHIR, Microsoft FHIR Server for Azure, Firely Server | The backend engine that stores, manages, and exposes FHIR data via a RESTful API. This is the core of your infrastructure. |
| Testing & Sandboxes | Inferno, Synthea, Public Sandboxes | Validating conformance to FHIR profiles (like US Core) and generating realistic (but synthetic) patient data for testing. |
| Development Libraries | HAPI FHIR (Java), fhir.js (JavaScript), FhirClient (.NET) | SDKs and libraries that simplify interacting with a FHIR server, handling serialization, and building FHIR resources in code. |
| Validation & Tooling | FHIR Shorthand, Sushi, Simplifier.net | Tools for creating and validating FHIR profiles and Implementation Guides, ensuring your data structures are correct and consistent. |
This is just a starting point, but having a solid FHIR server, a good testing framework, and the right development libraries forms a powerful foundation for any project.
Keep a Watchful Eye with Monitoring and Logging
Your job isn’t done when the system goes live. In fact, it’s just beginning. Continuous monitoring and logging are your eyes and ears, giving you real-time insight into how your system is performing in the wild. You need to be tracking key metrics to spot trouble before it impacts your users.
At a minimum, you should be watching:
-
API Latency: How long does it take your server to respond? Keep an eye on the average and the 99th percentile to see the worst-case user experience.
-
Error Rates: What percentage of API calls are failing? A sudden jump is the clearest sign that something is wrong.
-
Throughput: How many requests per minute is your system handling? This helps you understand usage patterns and plan for future capacity needs.
Tools like Prometheus, Grafana, and the ELK Stack (Elasticsearch, Logstash, Kibana) are fantastic for this. They allow you to build dashboards and set up alerts that can notify your team when a metric crosses a critical threshold. This proactive approach means you can often diagnose and fix an issue before a single user even notices.
The Future of Interoperability with FHIR and AI
A solid FHIR integration strategy isn’t just about connecting systems; it’s about laying the groundwork for the next wave of healthcare innovation driven by artificial intelligence. When you convert fragmented, proprietary data into a standardized, machine-readable format, FHIR becomes the high-octane fuel for sophisticated AI and machine learning models. This is where the future of intelligent, proactive healthcare is being built right now.
The possibilities are genuinely exciting. Think about predictive analytics models ingesting real-time public health data through FHIR APIs to forecast disease outbreaks with stunning accuracy. Or picture AI-powered clinical decision support tools, baked right into the EHR, pulling a patient’s complete history via FHIR to deliver personalized treatment recommendations in seconds. This isn’t science fiction; it’s the real-world outcome of a smart FHIR strategy.

Unlocking Advanced AI Capabilities
FHIR is on a clear path to becoming the API standard for healthcare. Projections show that we’re about to hit a critical mass, with 71% of organizations expected to use it by 2025, climbing toward 80% by 2026. This widespread adoption is what will truly unlock the integration of AI, telehealth, and IoMT in a digital health market poised to blow past $300 billion.
This standardized data access is the key to training and deploying AI that actually works in a healthcare setting. When your models are fed clean, consistent data, they can do some incredible things:
-
Automating Diagnostics: AI can analyze medical images like X-rays or MRIs, cross-referencing them with FHIR-based patient records to spot anomalies faster and more accurately than a human ever could.
-
Personalizing Treatment: You can develop algorithms that predict how a patient will respond to different therapies based on their unique genetic, clinical, and lifestyle data – all pulled together through FHIR.
-
Optimizing Operations: Machine learning can analyze hospital workflow data to predict admission rates, helping to optimize everything from bed management to staff scheduling.
As you explore the intersection of FHIR and the advantages of AI for your business, it’s also worth looking into how advanced tools like Large Language Models (LLMs) are shaping the next generation of interoperability solutions.
FHIR isn’t just about connecting today’s systems anymore. It’s about getting your organization ready for the intelligent, data-driven healthcare of tomorrow. A proactive FHIR strategy is the most important step you can take toward becoming a leader in the digital health era.
Tapping into this potential requires real expertise. By working with a team that has a deep understanding of AI development services, you can start building the solutions that will define the future of medicine.
Frequently Asked Questions About FHIR Integration
Diving into a new standard like FHIR always kicks up a few questions. It’s a big shift for any organization. Let’s tackle some of the most common ones we hear from teams just getting started.
What’s the Single Biggest Hurdle in a FHIR Project?
Honestly? It’s the data. Not the technology, not the APIs, but the raw data itself.
The real challenge lies in mapping your existing, often proprietary, data formats over to the standard FHIR Resources. This isn’t just a technical task; it demands a deep understanding of the clinical or administrative meaning behind the data. You have to ensure semantic interoperability, making sure the receiving system understands the meaning, not just the structure. This is where most projects get bogged down, and where having a team that’s been through it before, especially one with a background in healthcare software development, really pays off.
How Is FHIR Really Different from Old-School HL7 V2?
Think of it as the difference between email attachments and a modern, interactive web app.
HL7 V2 is message-based. You get a big, clunky block of text that you have to parse line-by-line. It works, but it’s rigid and painful for developers. FHIR, on the other hand, is built on the same tech that powers the modern internet: RESTful APIs and JSON.
Instead of parsing a massive message, a developer can just ask for what they need, like pulling up just the patient’s allergies. This resource-based model makes FHIR far more intuitive, faster to work with, and a natural fit for today’s web and mobile applications.
The game-changer with FHIR is its modern, API-first design. It was built for the internet, enabling a kind of plug-and-play interoperability that was simply a dream with older standards.
Does FHIR Only Handle Clinical Stuff?
Not at all. While its roots are firmly in clinical data, think patient records, lab results, and medications, FHIR is incredibly flexible.
Its design allows it to be extended well beyond the clinic. We’re seeing it used for all sorts of things:
-
Administrative data, like patient registration
-
Financial information, such as claims and billing
-
Public health reporting and research data
This adaptability is a huge part of why FHIR is gaining so much traction. It’s becoming the common language for the entire healthcare ecosystem, not just one part of it.
Okay, I’m Sold. Where Do I Even Begin?
Don’t try to boil the ocean. That’s the fastest way to get overwhelmed.
Pick one, specific, high-value problem you want to solve. Maybe it’s connecting a single new app or streamlining a particular data exchange between two systems. Start there. Get your hands dirty using public FHIR test servers and sandboxes; they’re perfect for experimenting without any risk. A successful pilot project builds incredible momentum and proves the value to the rest of the organization. Then you can scale.
Ready to build the future of connected healthcare? At Bridge Global, we specialize in crafting secure, scalable, and intelligent software solutions. Partner with us to accelerate your FHIR integration and unlock the full potential of your health data. Explore our custom software development services and let’s build something remarkable together.



