A Guide to Choosing Patient Engagement Platforms
The days of one-off appointments and stacks of paper files are quickly becoming a thing of the past. In their place, patient engagement platforms are reshaping healthcare, turning it from a series of disconnected events into a continuous, collaborative journey. Don’t think of these platforms as just another piece of software; they’re more like the central nervous system connecting patients and providers in real time.
The New Era of Connected Patient Care
We’re seeing a fundamental shift in healthcare, moving away from a model of reactive treatment toward one of proactive, continuous care. This change directly addresses long-standing problems like communication gaps, crushing administrative burdens, and low patient adherence. The goal is to turn passive patients into active participants in their own health journey. Innovations like chatbots in healthcare are a big part of what’s making this new era of connected medical services possible.
This digital evolution creates a more connected care model where everyone wins. For patients, it means instant access to their health information, direct communication with their care teams, and personalized educational content that helps them truly understand and manage their conditions.
For providers, the benefits are just as significant. It means a smoother, more efficient workflow. Automated reminders slash no-show rates, secure messaging ends the frustrating game of phone tag, and digital data collection frees up precious time to focus on what matters most – caring for patients.
The Core of the Transformation
At its heart, this shift is all about using technology to build stronger patient-provider relationships. It’s about making sure the care and support continue long after the patient has left the clinic. These platforms make that happen by providing the right tools for the job:
-
Continuous Communication: Secure messaging, telehealth visits, and automated check-ins keep the lines of communication open and easy.
-
Accessible Education: Delivering tailored content helps patients grasp their conditions and treatment plans, which in turn boosts adherence.
-
Empowered Self-Management: Tools for tracking symptoms, medications, and vital signs give patients a hands-on role in managing their health.
-
Streamlined Administration: Digital appointment scheduling, online form completion, and simple bill pay reduce the administrative headache for everyone involved.
This digital partnership is essential for thriving in a value-based care world. When patients are more engaged, clinical outcomes improve, satisfaction scores rise, and the overall cost of care can be reduced.
Putting together these sophisticated systems requires a deep well of expertise. As an experienced AI solutions partner, we know that building a successful platform is about more than just slick technology; it’s about designing systems that genuinely improve both the patient experience and clinical results. This forward-thinking approach ensures your organization is ready for the future of connected healthcare.
What Makes a Great Patient Engagement Platform Tick?
So, what’s the real difference between a basic patient portal and a platform that genuinely drives engagement? It’s all in the architecture. We’re moving away from a passive, digital filing cabinet to a dynamic, interactive “healthcare command center” for the patient. A high-performing platform isn’t just a random list of features; it’s a thoughtfully designed ecosystem where every piece works together to empower patients and lighten the load for clinical teams.

Think of it like building with LEGO bricks instead of carving a statue from a single block of stone. The best platforms use a modular and scalable design. This approach lets a healthcare organization start with the essentials and then click new modules into place as their needs change and grow. That kind of flexibility is a hallmark of expert custom software development, which always favors long-term adaptability over rigid, one-size-fits-all products.
The Four Pillars of Engagement
While the bells and whistles can vary, every truly effective platform is built on four non-negotiable pillars. These are the functional foundations that make meaningful interaction possible and lead to better health outcomes. Without them, a platform is just a digital brochure.
-
Secure Communication Channels: We’re talking about more than just a simple messaging system. This includes HIPAA-compliant messaging for one-on-one chats between patients and providers, broadcast tools for public health updates, and automated reminders for pre- and post-visit care.
-
On-Demand Health Information Access: Patients need 24/7 access to their own health records. This means lab results, medication lists, visit summaries, and immunization histories – all presented in a way that’s actually easy to understand.
-
Intelligent Self-Service Tools: This pillar is all about making administrative tasks easier for everyone. Features like online appointment scheduling, digital intake forms, and integrated bill pay drastically cut down on staff busywork and create a much smoother experience for patients.
-
Integrated Telehealth Capabilities: Conducting a virtual visit shouldn’t require a separate app. The ability to launch a video call directly within the platform is now a standard expectation. This keeps everything and all the data in one secure, convenient place.
A truly high-performing platform knits these pillars into a single, seamless user experience. The goal is to make managing your health feel as intuitive as managing your finances with a modern banking app.
Beyond the Basics: Essential Features That Drive Results
Building on these core pillars, the best platforms add features that actively guide patients on their care journey. An effective patient engagement platform doesn’t just show data; it provides context and tools. This is where we see huge improvements in treatment adherence and outcomes, backed by research showing that digitally engaged patients often have quicker recoveries and fewer complications.
This is precisely why a deep understanding of healthcare software development is so crucial. It’s about building systems that are not just technically solid but also empathetic to both the patient’s needs and the provider’s workflow. As an experienced AI solutions partner, we see it every day: thoughtful architecture leads directly to better adoption and more powerful results.
The table below breaks down some of these essential features and the real-world impact they have.
Essential Features of Modern Patient Engagement Platforms
This table categorizes and explains the core functionalities that healthcare organizations should prioritize when evaluating a patient engagement solution.
| Feature Category | Core Functionality | Impact on Patient/Provider |
|---|---|---|
| Care Plan Management | Interactive checklists, medication reminders, and progress tracking tools. | Patients feel more in control of their treatment, leading to better adherence. Providers gain real-time insight into patient progress between visits. |
| Personalized Education | Delivers articles, videos, and resources based on a patient’s specific diagnosis or upcoming procedure. | Increases patient health literacy and confidence. Reduces provider time spent on repetitive explanations. |
| Remote Patient Monitoring | Integrates with wearables and home medical devices (e.g., glucose meters, blood pressure cuffs). | Allows for proactive management of chronic conditions. Providers can intervene early based on real-time data alerts. |
| Data & Analytics | Gathers and analyzes patient-reported outcomes and engagement metrics. | Provides actionable insights to improve care quality. Helps organizations meet regulatory requirements and demonstrate value. |
Ultimately, the anatomy of a superior platform is all about its ability to create a proactive partnership. It transforms healthcare from a series of disconnected appointments into a continuous, supportive conversation between patients and their providers.
How AI Is Making Patient Engagement Smarter
Artificial intelligence is what’s turning today’s patient engagement platforms from basic communication tools into something far more powerful: predictive, personalized health partners. It isn’t about replacing the human touch in medicine. Far from it. The goal is to enhance it, making every interaction more insightful and effective by spotting patterns in health data that humans simply can’t.

This layer of intelligence takes a platform’s capabilities way beyond simple appointment scheduling and secure messaging. It’s what allows healthcare providers to get ahead of problems, shifting from reactive care to proactive health management. We’re talking about anticipating a patient’s needs before they snowball into something serious. These capabilities are a direct result of specialized AI development services.
Predictive Analytics for Proactive Care
One of the biggest wins for AI in this space is its ability to identify at-risk patients early. Machine learning models dig through data from EHRs, wearable devices, and patient surveys to flag individuals who might be heading for a hospital readmission, struggling with their medication schedule, or at risk of complications from a chronic disease.
Think of it this way: an algorithm might notice a patient with diabetes has consistently high glucose readings just as their step count from their fitness tracker drops off. Instead of waiting for the next appointment, the system can automatically alert a care manager. That manager can then jump on a quick telehealth call or send some helpful articles about diet and exercise.
This predictive power fundamentally shifts the focus from treating sickness to maintaining wellness. It lets care teams put their time and energy where it’s needed most, right at that moment.
This isn’t just some futuristic idea; it’s happening now, and it’s improving outcomes. When a clinical team can see a potential problem on the horizon, they can step in to prevent it. That’s better for the patient and a lot more cost-effective for the health system.
Personalization at Scale
Let’s be honest, generic health advice usually goes in one ear and out the other. AI flips the script by making hyper-personalization possible, delivering the right information to the right person at exactly the right time.
So, instead of every post-op patient getting the same PDF recovery guide, an AI-driven platform can customize it. The information will be tailored based on their specific surgery, age, other health conditions, and even whether they prefer to watch a video or read an article. This approach makes the guidance feel relevant and, more importantly, makes it much more likely to be followed.
Here’s how this plays out in the real world:
-
AI Chatbots: These smart assistants offer 24/7 support. They can answer common questions, guide patients through the app, or even help triage symptoms to see if a human clinician needs to get involved. As we’ve covered before, these tools are a game-changer for patient access, a topic we explore more in our guide on the role of healthcare AI chatbots.
-
Content Curation: The platform can analyze a patient’s health profile and automatically suggest relevant articles and videos. This helps boost their health literacy and keeps them actively involved in their own care.
-
Behavioral Nudges: Based on a patient’s unique care plan and past actions, the system can send timely, encouraging reminders to take medication, do their physical therapy exercises, or book a follow-up visit.
Automating Workflows and Reducing Burnout
Finally, AI is a massive help in easing the administrative load that weighs down clinicians and contributes to burnout. By automating the routine stuff, AI gives doctors, nurses, and their teams more time to focus on what they do best: caring for patients.
Here are a few examples of smart automation in action:
-
Predicting No-Shows: AI models can analyze past appointment data to flag patients who are likely to miss a visit, giving staff a chance to send an extra reminder or offer to reschedule.
-
Intelligent Triage: AI can scan incoming patient messages, flagging urgent requests for immediate attention while routing billing questions or prescription refills to the right administrative person.
-
Data Summarization: Before a visit, an advanced algorithm can create a quick, digestible summary of the patient’s recent activity, vitals, and reported symptoms, so the clinician is up to speed in seconds.
By making patient engagement smarter, AI doesn’t just create a better experience for the patient. It helps build a more sustainable, efficient, and effective healthcare system for everyone.
Navigating Compliance and EHR Integration
When you’re looking to bring in a new patient engagement platform, it’s easy to get caught up in all the shiny features. But let’s be honest, the real heavy lifting happens behind the scenes with security and system integration. These aren’t just boxes to check; they are the absolute foundation of a successful and legal implementation.
Get this part wrong, and even the most impressive platform becomes a massive liability.
First and foremost is airtight data security and strict HIPAA compliance. The trust between a patient and their provider is everything, and that trust has to extend to how you handle their digital information. Understanding HIPAA essentials for clinicians isn’t just for the compliance department; it’s crucial for anyone involved. Every single piece of data, from a basic appointment reminder to sensitive lab results, must be encrypted at all times, whether it’s sitting on a server or moving across the network.
The EHR Is Still the Single Source of Truth
A patient engagement platform can’t operate on an island. To be truly effective, it has to connect seamlessly with your organization’s Electronic Health Record (EHR) system. Think of the EHR as the clinical heart of your operations; it’s the official, single source of truth for all patient medical data.
When a platform is disconnected from the EHR, you get data silos. This leads to confusion, potential errors, and a frustrating, fragmented experience for everyone involved. Patients get mixed messages, and clinicians waste time trying to reconcile conflicting information.
The integration acts like a sophisticated two-way conversation. When a patient books an appointment in the app, it should instantly pop up in the EHR schedule. When a doctor adjusts a prescription in the EHR, that update should immediately appear in the patient’s portal. This constant, reliable communication is what keeps the patient’s record consistent and accurate across the board.
This drive for connected systems is what’s behind the explosive market growth. The global patient engagement solutions market is expected to jump from USD 29.33 billion in 2025 to USD 51.69 billion by 2030. This surge isn’t just about new apps; it’s about the deep integration of these platforms into the core EHR infrastructure. Learn more about the market growth from these findings.
Bridging the Gap With Interoperability Standards
So, how do you get these different systems to talk to each other? You need to speak the same language, and in healthcare IT, that means using established interoperability standards.
Interoperability isn’t just a technical goal; it’s a clinical imperative. It’s what ensures the right information gets to the right person at the right time, preventing dangerous gaps in care.
There are two primary standards you’ll encounter:
-
HL7 (Health Level Seven): This is the classic, workhorse standard for exchanging clinical and administrative data. It’s been the bedrock of healthcare data exchange for decades.
-
FHIR (Fast Healthcare Interoperability Resources): FHIR is the modern evolution, built on the web technologies that power today’s internet. It’s far more flexible and developer-friendly, making it perfect for mobile apps and cloud-based platforms.
Navigating HL7 and FHIR integrations can get complicated fast, which is why partnering with an experienced technology team is so important. A good partner can design an integration that actually improves your clinical workflows instead of creating new headaches. For a deeper dive, as we explored in our guide, you can learn about the key benefits of EHR integration services.
By putting compliance first and building a solid, reliable bridge to your EHR, you’re creating the secure, connected environment necessary for a patient engagement platform to truly succeed. This is the groundwork that makes better patient outcomes and stronger provider collaboration possible.
Your Roadmap to a Successful Platform Rollout
A powerful platform is one thing, but making it work in the real world is another. Even the most advanced patient engagement platforms will fall flat if the rollout is rushed or disorganized. To get it right, you need a clear, step-by-step roadmap that ensures a smooth transition, keeps daily operations running, and gets everyone on board from day one.
This journey starts long before you even think about signing a contract. The first, most critical step is a thorough needs assessment. This means getting everyone in a room: clinicians, front-desk staff, and even a patient advisory council, to get to the heart of your organization’s biggest headaches. Are you battling high no-show rates? Struggling to help patients with chronic conditions stick to their medication schedules? Or just trying to free up staff from endless administrative phone calls?
When you define these goals upfront, you create a practical scorecard for evaluating different solutions. It helps you cut through the marketing noise and pick a platform that genuinely solves your specific problems.
Building Momentum with a Phased Rollout
Tempting as it might be, a “big bang” launch where everything goes live at once is a recipe for chaos. A much smarter strategy is a phased approach, usually kicking off with a Minimum Viable Product (MVP). An MVP isn’t the entire platform; it’s just the essential features needed to solve one key problem for a select group, like a single department or a specific patient population.
This method pays off in several ways:
-
Quick Wins: A successful pilot creates buzz and turns early users into your biggest advocates, building momentum for the full rollout.
-
Real-World Feedback: You get to hear what a smaller, controlled group of users really thinks, allowing you to fine-tune the platform before it goes wide.
-
Lower Risk: It keeps the initial investment and complexity in check, making the whole project feel much more manageable.
Once that pilot is a proven success, you can start rolling out more features and adding more users in carefully planned stages. This iterative process means every new function is introduced with the right training and support. Our experience shows that this kind of structured, expert-led implementation is the secret to hitting your strategic goals without derailing clinical workflows.
This diagram shows how a new platform has to fit into your existing systems while keeping everything secure.
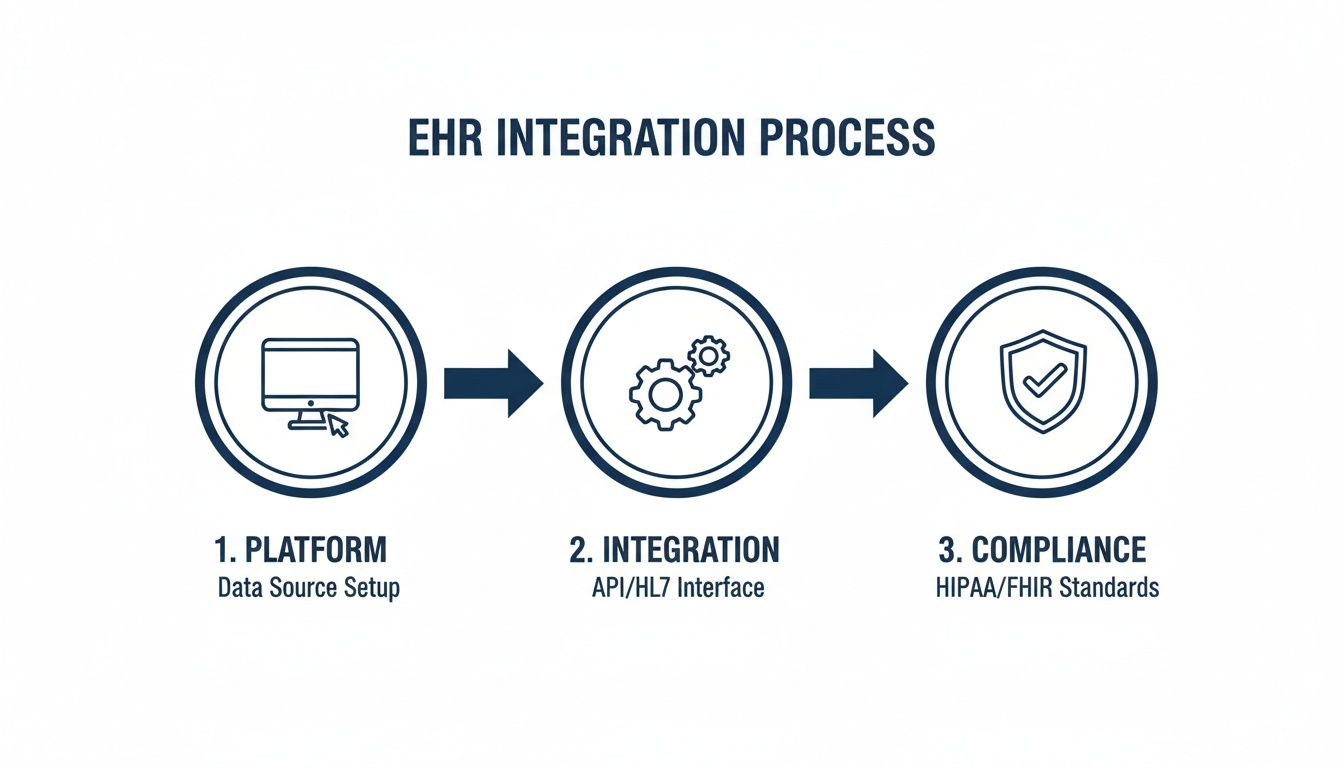
As you can see, the platform itself, its integration with your EHR, and ongoing compliance are all interconnected parts of a secure and functional system.
Driving Adoption Through Training and Change Management
Remember, technology doesn’t create change – people do. That’s why you can’t skimp on staff training. This needs to be more than a one-and-done webinar; think of it as an ongoing program that helps everyone understand not just how to click the buttons, but why this new tool makes their jobs easier and improves patient care.
At the same time, you need a plan to get patients to actually use it. A simple patient adoption campaign using email, signs in the waiting room, and encouragement from your team can make a huge difference. Point out the clear benefits, like the time they’ll save by scheduling online or getting quick answers through secure messaging, and you’ll see adoption rates climb.
The good news is that modern cloud-based solutions have made implementation far less painful. In fact, these platforms are on track to capture a massive 69.62% market share by 2025. This industry-wide shift away from clunky, on-premise systems highlights the need for flexible, accessible tools that let providers connect with patients anywhere.
At the end of the day, a successful implementation is all about managing change. As we’ve explored in our guide to the principles of digital health platform engineering, a well-executed plan ensures your new platform becomes an essential, valued part of how you deliver care.
Measuring What Matters: Calculating Your ROI
So you’ve decided to invest in a new patient engagement platform. It’s a big move, and a smart one, but how do you prove it’s actually working? To build a solid business case, you have to look past the fluffy metrics and get down to the Key Performance Indicators (KPIs) that really move the needle. It’s all about drawing a straight line from the platform’s features to real-world clinical and financial results.
A great platform does more than just boost patient satisfaction surveys. It makes your entire healthcare system run smoothly and more effectively. The end game is to calculate a concrete Return on Investment (ROI) by tracking specific, measurable improvements across the board.
Key Performance Indicators to Track
To get a true read on your success, you need a balanced scorecard. Think of it in three buckets: clinical outcomes, operational efficiency, and patient satisfaction. Together, these metrics paint a full picture of the platform’s impact.
Here are the essential areas to keep your eyes on:
-
Clinical Outcomes: This is where the rubber really meets the road. Are you seeing reduced hospital readmission rates for high-risk conditions like heart failure? Are you tracking improvements in chronic disease markers, like better A1c levels for your diabetic population?
-
Operational Efficiency: How much administrative drag is the platform eliminating? Watch for things like lower appointment no-show rates, a noticeable drop in routine phone calls to your front desk, and quicker patient intake and registration times.
-
Patient Satisfaction and Adherence: Of course, you want to see higher patient satisfaction scores (like HCAHPS). But also look for an uptick in appointment adherence and better completion rates for patient-reported outcome measures (PROMs) – collecting these digitally almost always boosts participation.
Measuring ROI isn’t just about cutting costs. It’s about proving that a more engaged patient community leads directly to better health outcomes, which ultimately drives long-term financial health for your organization.
Calculating Your Financial Return
Once you have a handle on the right KPIs, you can start putting dollar signs next to them. The calculation is a mix of direct cost savings, new revenue captured, and penalties avoided.
First, tally up the costs. It’s pretty straightforward:
-
Initial Investment: This includes your platform licensing, any implementation fees, and the cost of training your staff.
-
Ongoing Costs: Don’t forget the recurring subscription fees, maintenance, and support contracts.
Next, it’s time to quantify the gains:
-
Reduced Administrative Costs: Figure out the staff hours saved by automating scheduling or reducing phone tag, and translate that into salary savings. A 15% reduction in no-shows, for example, isn’t just a number; it’s directly recoverable revenue.
-
Lower Readmission Penalties: Calculate the hard dollars saved by staying below the national benchmarks and avoiding those hefty financial penalties.
-
Increased Revenue: Tally up the additional revenue you’re generating by filling appointment slots that used to be empty due to no-shows.
Subtract your total costs from your total financial benefits, and you’ve got a clear, data-driven ROI. This isn’t just about justifying the upfront check you wrote; it’s about showcasing the lasting financial power of building a healthier, more connected patient community through smart healthcare software development.
Frequently Asked Questions
Diving into the world of patient engagement platforms often brings up a few key questions. We’ve gathered some of the most common ones here to give you straightforward answers and help you find the right path for your organization.
Where Do I Even Begin When Choosing a Platform?
The absolute first step happens long before you ever see a product demo: a thorough internal needs assessment. You have to know what you’re trying to fix before you can find the right tool. Are you trying to cut down on no-shows? Make chronic care management less of a headache? Or just give your staff a break from mind-numbing administrative tasks?
Get your key people in a room: clinicians, front-desk staff, administrators, even patient advocates, and hammer out a prioritized list of “must-have” features. This foundational work gives you a clear scorecard for evaluating vendors. It’s the only way to ensure the platform you choose actually solves your real-world problems, a principle we’ve seen play out in our various client cases.
How Do These Platforms Keep Patient Data Safe and HIPAA Compliant?
This is a big one, and rightfully so. Trustworthy platforms are built from the ground up with a multi-layered security strategy. Think of it like a bank vault with several locks. They use end-to-end data encryption, host data on secure, HIPAA-compliant cloud services, and enforce strict role-based access so people can only see the information they absolutely need to. Following all HIPAA safeguards isn’t optional; it’s the bare minimum, proven by regular, independent security audits.
When you’re talking to a potential vendor, ask to see their compliance certifications and their data breach response plan. A solid partner who specializes in healthcare software development won’t just treat compliance as a final checkbox; it will be woven into their entire development process.
Can a New Platform Actually Work With Our Existing EHR System?
Yes, it has to. In fact, if it can’t, it’s a non-starter. Modern patient engagement platforms are designed to play well with others, using standard communication protocols like HL7 and FHIR to talk to different EHR systems. This connection is what allows data to flow smoothly and in real-time between systems, which means no more duplicate records and a single, consistent source of truth for both patients and providers.
Pulling off a seamless integration often takes an experienced technology partner who knows how to navigate the tricky parts of connecting disparate systems. This ensures your data stays clean and the experience is smooth for everyone. If you want to understand more about integrating complex systems, our guide on approaching AI for your business offers some great insights.
Ready to build a smarter, more connected healthcare experience? As a leading AI solutions partner, Bridge Global specializes in creating secure, scalable, and intelligent patient engagement platforms. Let’s build the future of healthcare together. Get in touch with our experts today!



